Swallow Study & NICU Visit ~ April 11th:
Emma got her swallow study done at Arnold Palmer hospital. I don't have any pictures from that since only one parent can go back at a time, so Michael took her and I waited in the Radiology lobby. It was nice to see that her original NICU Speech Therapist, Michelle, was the one doing this test. Emma passed and showed that she was able to swallow formula and some baby food without aspirating. A copy of the study was sent to the current Speech office, so Christine (the speech therapist who comes to our house twice a week) could start giving Emma baby food and applesauce when she is here. Sometimes if Emma is having a crabby time- usually if she happens to need her nap at that time, unlike today where she is napping at Noon, which is great so she'll be awake and happy for therapy at 3pm- then Christine will just read to her and play with bubbles instead of trying to feed her.
After the study, Michelle urged us to visit the NICU since we hadn't been back since Emma was discharged on April 30th, 2018. Michael said it could be up to me whether we visit, which I was surprised by since he hates the security system at the front. The metal detector always beeps when he goes through because of his belt and the security guards basically make him take his shirt off to prove he doesn't have anything else on him. I voted for yes to visiting since it had been almost a year since a lot of the staff had seen Emma in person. Many of them keep in contact via social media, but we found that one of her main doctors, Doctor Lipman, had retired recently and one of her respirator therapists, Errica, had left and gone back to school.While we were there we saw a lot of people, many more than in the photos (including Maureen/ "Mo"- one of Emma's nurses at the beginning, Cori- a Nurse Practitioner, and Dana- her NICU physical therapist) and I wish we had gotten a picture with everyone, but it was so nice to see them. One of the girls was telling us about a gala that is happening in June (next weekend, while I'll be working) for a non-profit that is starting up called Matthew's Gift. She recently told me that Matthew's parents have heard all about us and Emma and offered to pay our tickets so we could go, but I'm training someone at work all of June, so I'm not able to get any days off. That was so sweet of them! When I said we wouldn't be able to make it, she also told me that they do a zoo event in November, so hopefully the weather is nice and I'm off so we can go to that! I'd really love us to take Emma to the zoo. She seemed to enjoy the aquarium when we went last summer.
Gore/Wilder Family Gathering ~ Mid April:
Michael's family came down for about five days because every year his dad and older brother, Christopher, who are both doctors, have to attend conferences, so this year they picked going to Orlando that way they could also visit us! Since Michael's parents and my parents don't get to visit each other often (the previous time his parents were here at the beginning of December, my parents were on a cruise for their anniversary!), my parents made sure to come down for the day so they could spend time together. My parents did get to see Michael's mom and grandma for Emma's first birthday, but my dad hadn't seen Michael's dad since we lived in Birmingham for half of 2014!!
 |
| Emma modeling a hat my mom got her on their Myrtle Beach vacation! |
^^ Us with Christopher and his wife, Meredith.
Although we last saw them in July 2017 when Emma was a month old in the NICU, this was the very first time Christopher and Meredith had met Emma!! |
| I definitely need to mention that this photo was taken after work and it was Mis-Match day during Telecommunicator Week. I definitely wouldn't be dressed like this otherwise! :D |
First Dentist Appointment ~ April 25th:
(I definitely thought I had written about this part already..) Emma has had 18 teeth since December, so it was recommended by the pediatrician twice that we make a dentist appointment for her. Two of the main reasons he wanted us to go is because since Emma can't close her mouth all the way and she barely ever eats anything by mouth, she gets more air and such on her teeth and her front molars do look a little bit yellow although we brush her teeth every night. Also because we don't use fluoride water on her teeth, she needed to get a fluoride cleaning done. The dentist was very nice and did really well with her. Plus we always love when doctors tell us how great of a job we are doing with her! Emma did seem to prefer to sit up in the chair, but in order for the dentist to be able to see her top teeth clearly, she was put on a soft board that was balanced on Michael's and the dentist's legs. She cried during that part when he had his gloved fingers in her mouth (she doesn't like it when the speech therapist does it either) and he rubbed the fluoride paste on her teeth with a Q-tip swab, but then she was fine after and got her Princess Belle toothbrush. She also got her name written on the "No Cavities" board. Hooray!!! We were told that she doesn't need to go back until next April.
Other things that were going on in Emma's world last month ~
Although she got a smaller stemmed Mic-Key button (1.2mm) switched out in March, with her continued ab exercises, her stomach wall is thinner, so there is space between her skin and the button. We bought these cute unicorn snap patches from Etsy, which help absorb any formula leakage. Michael designed and 3D printed the purple piece, although the day after I took this photo, he made a better version which is gray. He calls it the G-Lock. (You can see the gray version in the photo at the bottom where Emma is laying on the couch.) He made it because Emma was found being able to disconnect the G-tube from the Mic-Key button. A few different times I saw her holding it and laughing while the formula continued to drip out around her! So this piece has been great to keep it secure. Once again, Bravo, Michael!! We recently ordered more unicorn patches since we put a new one around her button each night.
Reading ~ April 7th: Back when I was doing a good job of bringing home lots of kid books from the library to read to Emma during the 15 minutes while her lung treatments are being done. I really need to get back on that! I really liked this "Smile A Lot" book by Nancy Carlson. It was just a really nice book about smiling even when bad things happen because it will make you happier and your life will be better. It really just seemed like an awesome book for Emma! She's so great about smiling a lot. :)
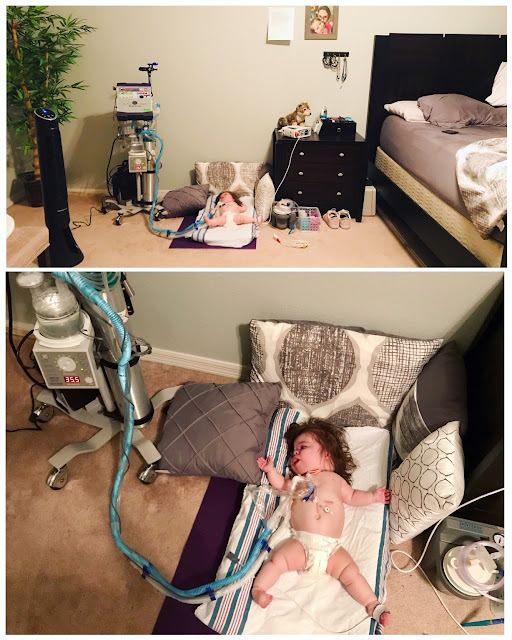
One day (April 11th) when we were practicing sitting again - while holding objects!! She has a sodium chloride bullet in each hand. Not long ago she would fall back if Michael simply wiped some drool from her mouth. Now she can counter balance while being tickled or lightly pushed from either side. It's a trick they use during therapy, but I can't remember what Lara called it.
Emma's "knee" flexion has been looking really good lately. (I put knee in quotes since part of her Meier-Gorlin Syndrome genetic condition is that she does not have kneecaps.)
Below: during Speech therapy, Christine working Emma's cheek muscles. I laughed when I told her that I have been squeezing Emma's cheeks together so she makes a silly face, but she told me that's actually good for her oral practice!
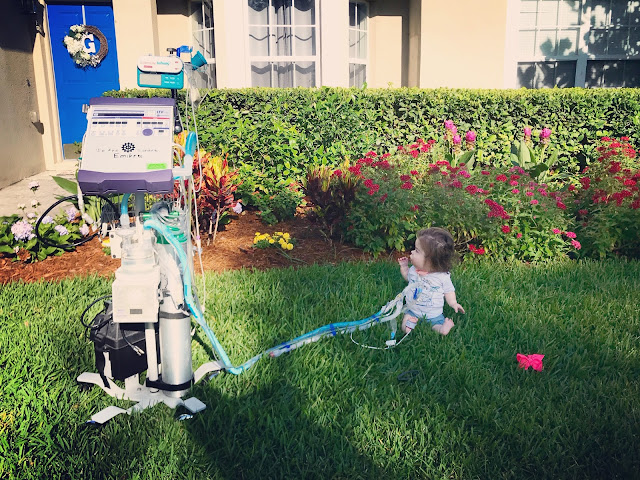
Emma testing out her new swing (April 20th). We have only tried it once so far because it has been ridiculously hot outside recently. Everyone has been posting pictures of their 100+ temperatures from their vehicle dashboards (in May). The other day Emma even got sweaty in the two minutes between rolling her out of the house to putting her in the car that had the 60 degree AC on full blast.^^ This is how Emma and I spend most of my days off: being lazy and watching Netflix, haha!!
She's such a happy girl and in this last photo you can see a aqua colored tube by where her hand is. That is the Passy Muir Valve (speaking valve) which we have been putting on her more lately. She has been very vocal without it, but when she wears it, it helps more air pass through her vocal cords, and she needs that practice to feel how she would breathe without the ventilator. Most kids without ventilators have a Passy Muir Valve on the end of their trach. It also allows for the senses of taste and smell, so she always wears it when we practice eating/swallowing.
We have a lot of therapy homework that we need to do better about keeping up with. I'll have to make a chart to keep us accountable! Making sure she's always wearing her glasses (and that the lenses are clean- since she's always rubbing her fingers on them when she tries to pull them off), wearing her leg splints most of the time, wearing the Passy Muir Valve often, feeding her baby foods while we all eat dinner together, sitting up more/ timing her balancing, arm and leg bending exercises since she only has Physical Therapy once a week for 30 minutes, reading books to her and showing her the pictures, as well as sign language for a handful of words we actually use daily ~ "Good job" is the one I'm working on the most right now. I know it's not the official sign, but I'm having her associate those words with clapping. I'll clap my hands and then clap her hands together, both while saying, "Good job!" in my happy voice.